Author: Jennifer Austin (BSc MS)
Understanding a condition like Lymphedema can be difficult due to the sheer amount of information available on the subject.
Here we will break down information on the condition into a more easily digestible form.
Let’s get right to it with an overview on Lymphedema.
What is Lymphedema?
Lymphedema refers to swelling that occurs in your limbs.
Usually it affects one of your arms and legs, however both arms and legs can get affected.
Lymphedema results from any blockage to your lymphatic system which prevents lymphatic fluid from draining.
It is not a curable illness, but the good news is it can be managed well by early diagnosis and proper care of the affected limb.
What are the causes of Lymphedema?
Your lymphatic system belongs to the immune system, which keeps your body healthy.
Lymphatic fluid which drains throughout your body is rich in proteins.
During circulation it collects germs (bacteria and viruses) and waste products and flows within the lymph vessels to lymph nodes which are situated in various sites in your body.
The lymphocytes (infection fighting cells that reside within your lymph nodes) filter the waste products and germs and flush them off your body.
Lymphedema occurs when your lymph vessels do not drain the lymphatic fluid adequately from your limbs.
When lymphedema occurs on its own causing improper drainage, it is called primary lymphedema.
This can be inherited where there are problems in development of lymph vessels in your body.
When there is an underlying condition causing damage of lymph vessels leading to blockage, it is called secondary lymphedema.
This is more common than the primary form.
The underlying conditions or diseases leading to blockage causing secondary lymphedema are:
Cancer – When cancer spreads, the cancer cells can block your lymph vessels especially when the tumor is growing near your lymph nodes or lymph vessels.
Radiation treatment for cancers – The radiation can lead to inflammation and scarring of any nearby organs or tissues along with destruction of tumor cells. Therefore, the nearby lymph vessels can get damaged due to the radiation therapy.
Infection – Lymph nodes can sometimes get infected which can block the flow. There are certain parasites like Filaria which can block the flow of lymphatic fluid.
This type usually occurs in one leg sometimes becoming massive (elephantitis). Infection related lymphedema is more common in tropical and subtropical countries.
Following certain surgeries – Some surgeries can injure lymph vessels and nodes leading to lymphedema.
In some instances the lymph nodes are removed to check for spread of cancer. For example in breast cancer patients, the lymph nodes which are suspicious of spread in the axilla (underarm) are removed.
This in turn blocks the lymphatic fluid flow leading to lymphedema of that particular arm.
Obesity and older age are risk factors towards developing lymphedema.
What are the stages of Lymphedema?
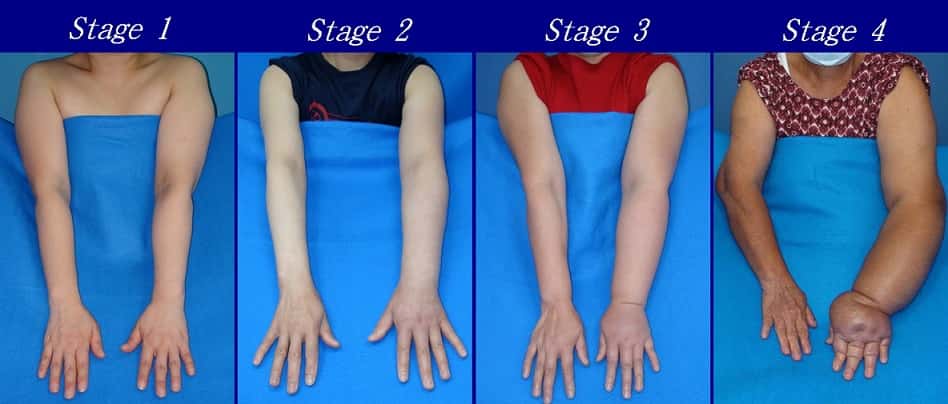
Lymphedema is a progressive disease which develops in stages.
These stages are categorized according to the severity.
Stage 0 – Latency stage
In this stage the transport of lymphatic fluid is impaired. Swelling is not evident; therefore it is in subclinical stage. This stage can exist for months or even years before edema or the swelling becomes evident.
Stage 1 – Mild stage
Fluid which is relatively high in protein is accumulated in the limb. However, since it is in early stage, elevation of the limb subsides the swelling. When pressed on the swelling pitting can occur. The proliferating cells are in increased numbers during stage 1.
Stage 1 and 2 are the reversible stages of lymphedema.

Stage 2 – Moderate stage
In this stage the limb elevation alone cannot reduce the swelling. Usually pitting doesn’t occur. The fibrosis of tissue starts to develop during this stage.
Stage 3 – Lymphostatic Elephantiasis stage
Pitting is absent in this stage. Trophic skin changes occur in the swollen limb such as; fat deposition, acanthosis and warty overgrowths.
What are the symptoms of Lymphedema?
Lymphedema can occur in any one or more of your arms and legs. The symptoms include:
- Swelling of the affected limb – this includes your fingers and toes as well
- Pain and discomfort
- Feeling of tightness and heaviness of the limb
- Difficulty in movement and restriction of the range of motion
When lymphedema is long lasting, you can develop recurrent infections. The affected limb will be red and tender to touch.
Prolonged lymphedema can change the overlying skin making it thickened (fibrosis)
Lymphedema if not treated properly can lead to serious complications such as recurrent infections of skin (cellulitis) and infection of lymph vessels (lymphangitis).
Untreated chronic lymphedema can rarely lead to cancer (lymphangio-sarcoma).
These complications if not identified and treated on time, may be life threatening.
When should you see a doctor?
Whenever you notice persistent swelling in your arm or leg, seek treatment early.
Do not wait until complications occur. If you are an already diagnosed patient with lymphedema, seek immediate medical attention if your involved limb suddenly increases in size.
If you have not been diagnosed your doctor will order certain imaging tests like MRI scan, CT scan or Doppler Ultra sound scan to diagnose lymphedema especially when the swelling is not very obvious.
For severe Lymphedema you may be offered surgery such as removal of excess tissues, removal of lymphatic blocks by anastomosis or Lymph node transplants.
What are the treatment options available for lymphedema?
Exercise and elevation of the affected limb – This is useful during the reversible stages, as it helps the drainage of lymphatic fluid. However the exercises should not be strenuous.
Massage – massage when done according to the proper technique can encourage lymph fluid drainage.
Pneumatic compression and use of compression stockings – The pressure gradient across the limbs will help lymphatic fluid drainage.
Your lymphedema therapist will teach you how to do these simple techniques when caring for your condition.
How do you prevent or reduce the risk of Lymphedema?
It is your responsibility to take care of your affected limb without getting injured. Here are some home remedies which you can try when taking care of your affected arm or leg.
Always keep your affected limb clean and dry, especially in between your toes. When there is too much moisture in toe webs, they will be more prone to develop fungal infections.
Elevate your affected limb – this will be more helpful in reversible stages of Lymphedema. Elevation should be above the level of your heart.
Protect your affected limb from getting injured – Cuts, burns and scrapes can lead to infection. Do not use sharp objects unnecessarily. If you find it difficult to cut your toe nails, get help.
If your arm is affected by lymphedema, wear protective gloves while cooking and gardening to prevent injuries.
If you stich, wear a thimble to prevent needle stick injuries.
Diabetes – If you are a diabetic make sure that your blood sugar levels are controlled. Uncontrolled diabetes will make you more prone to infections such as cellulitis and fungal infections.
Blood drawing and vaccinations to your affected limb should be avoided unless really necessary.
Temperature Extremes – Avoid excessive temperatures like heating pads or ice packs on your affected limb. Extreme temperatures can damage the overlying skin of the affected arm or leg.
Clothing – Do not wear tight clothing as a swollen limb can get damaged or blood supply can get cut off. Tight clothing and blood pressure cuffs can constrict your limbs.
Rest – When recovering after a surgery, rest your limbs. Elevate affected limbs where possible.
Exercise – Following cancer radiotherapy exercise and stretching can be done according to the advice given by your physiotherapist.
You can start exercises gradually and build up slowly. Walking is a good way to start, if you haven’t exercised in a while.
Gradually increase the pace and distance of walking. You can also do yoga, cycling, jogging or swimming. However make sure that you dry your limb well with a soft cloth/ towel especially in between toes.

Control your diet – Avoid refined sugars, refined grains (especially gluten containing grains) and high salt foods like chips and French fries. Limit fat intake and animal products including dairy.
Avoid alcohol and smoking – alcohol causes expansion of blood vessels which in turn increase the amount of fluid which accumulates within the tissues.
In healthy individuals this excess fluid is removed by their lymphatic system. But in patients affected with lymphedema, this doesn’t occur.
Therefore, excessive consumption of alcohol can increase swelling of the affected limb.
Smoking can narrow your blood vessels which decrease the blood flow to your limbs and deplete the limb tissues of oxygen and nutrients.
Smoking can also damage elastic fibers and collagen which gives your skin the strength and elasticity. These stresses can worsen lymphedema.
Lose weight if you are obese or overweight – Some studies have shown that losing weight can significantly improve symptoms of lymphedema in individuals who are overweight.
Discuss with your doctor regarding a diet plan and a safe exercise routine to reduce your weight to a healthy level.
Inspect the skin of your affected limb daily – If your eye sight is weak, get help. Examining for early changes and breaks in your skin can prevent you from getting infection as you can seek treatment early for any change in your skin.
Injuries to skin invites infection to lymphedema affected limbs.
Never walk bare foot as your feet can get injured. Even a minor scratch can lead to infection in a limb affected by lymphedema.
We hope you have found this article useful and informative.
Check back with lymphedemalifeline.org for more articles like this.
Disclaimer – The information on this website is for informational purposes only. Lymphedemalifeline.org and it’s staff, writers, etc. assumes no responsibility for any consequences arising from any use made of, or any reliance on, the information contained on this website.

